Endometriosis and Its Link to Infertility
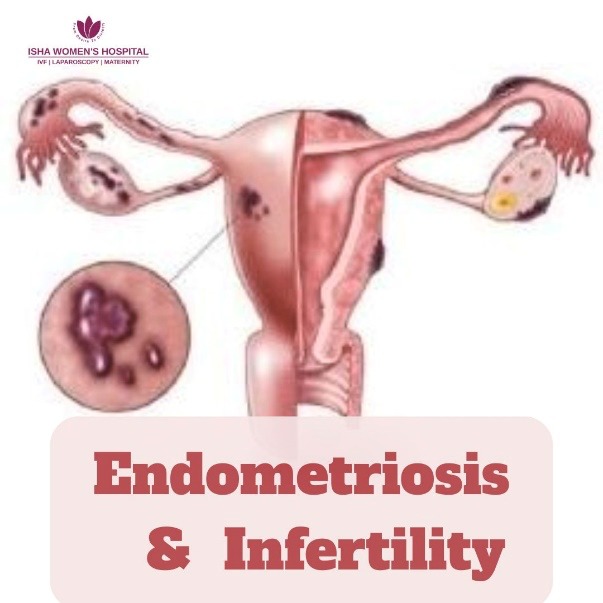
In endometriosis, tissue similar to the lining of the uterus begins to grow outside the uterus — commonly on the ovaries, fallopian tubes, bladder, and even the intestines. This misplaced tissue causes inflammation, scarring, and severe pelvic pain. But beyond discomfort, one of the most emotionally challenging aspects of endometriosis is its link to infertility.
In this blog, we will go through everything you need to know about endometriosis and its impact on fertility — from recognizing symptoms and getting diagn
What Is Endometriosis?
These abnormal growths are most commonly found on the:
- Ovaries
- Fallopian tubes
- Outer surface of the uterus
- Bladder
- Bowel or intestines
- And occasionally, in other areas of the pelvic cavity
- Chronic inflammation
- Formation of scar tissue (adhesions)
- Ovarian cysts (endometriomas)
- Severe pelvic pain and fertility problems
The condition primarily affects women of reproductive age, typically between 15 to 49 years old. However, some women are diagnosed earlier or later in life.
Causes & Risk Factors
- Retrograde Menstruation: This is one of the most widely accepted theories. During menstruation, some of the menstrual blood flows backwards through the fallopian tubes into the pelvic cavity instead of leaving the body. This backwards flow can deposit endometrial cells onto pelvic organs, where they implant and grow.
- Genetic Predisposition: Endometriosis tends to run in families, suggesting a genetic component. If your mother or sister has endometriosis, your risk of developing it is higher.
- Immune System Dysfunction: A weak or faulty immune system may fail to recognise and destroy misplaced endometrial tissue growing outside the uterus, allowing it to survive and spread.
- Menstrual and Hormonal Factors: Certain menstrual patterns and hormonal factors are associated with a higher risk:
- Early onset of menstruation (before age 12)
- Short menstrual cycles (less than 27 days)
- Heavy or prolonged periods
- Increased estrogen levels in the body
- Family History: Having a first-degree relative (such as a mother, sister, or aunt) with endometriosis significantly increases your chances of developing the condition
Signs and Symptoms of Endometriosis
Here's a breakdown of the most common signs to watch for:
- Pelvic Pain
- Most common symptom of endometriosis.
- Typically felt in the lower abdomen or back.
- Intensifies during menstruation.
- Not just regular period pain — it can be severe and ongoing.
- Pain During Sex
- Pain may be deep, sharp, or burning during or after intercourse.
- Often caused by endometrial tissue near or behind the vagina or uterus.
- Painful Periods (Dysmenorrhea)
- Menstrual cramps that are more intense than normal.
- Worsen over time and may not be relieved by typical pain medication.
- Bowel or Urinary Pain
- Discomfort or pain during urination or bowel movements, especially during periods.
- May indicate endometrial tissue affecting the bladder or intestines.
- May also be accompanied by diarrhea, constipation, or bloating.
- Fatigue
- Chronic pain and inflammation can cause extreme tiredness.
- Often leads to difficulty in managing everyday tasks.
- Infertility
- Endometriosis is a major cause of female infertility.
- Women may face difficulty in conceiving or experience repeated miscarriages.
- For some, infertility is the first sign of the condition.
How Endometriosis Is Diagnosed
Here are the common steps involved:
• Pelvic Examination: During a routine pelvic exam, your doctor may feel for abnormalities like ovarian cysts or thickened tissues behind the uterus. However, small endometrial implants are often not detectable this way.
• Ultrasound or MRI: Imaging tests like transvaginal ultrasound or MRI can help identify large endometriotic cysts (endometriomas) or damage to pelvic organs. However, these tests may not reveal small implants or adhesions.
• Laparoscopy (Gold Standard): A laparoscopy is a minor surgical procedure performed under anesthesia. A small camera is inserted through a tiny incision in the abdomen to directly view the pelvic organs.
This is the only definitive way to diagnose endometriosis. During this procedure, doctors can:
- Confirm the presence of endometrial tissue
- Determine its exact location and severity
- Sometimes remove or treat the lesions during the same surgery
Staging the Disease
- Stage 1 – Minimal
- Presence of a few small endometrial implants.
- Little to no scar tissue formation.
- Stage 2 – Mild
- Increased number of implants with deeper penetration.
- Slight formation of adhesions (scar tissue).
- Stage 3 – Moderate
- Numerous deep implants visible.
- Small cysts may form on the ovaries.
- Noticeable scar tissue is present.
- Stage 4 – Severe
- Extensive deep implants spread throughout the pelvic region.
- Large ovarian cysts may develop.
- Significant scarring and possible damage to pelvic organs.
The Link Between Endometriosis & Infertility
• Affects Egg Quality, Ovulation, and Fallopian Tube Function
Endometriosis can damage the ovaries, which are responsible for releasing healthy eggs. Inflammation or cysts (called endometriomas) on the ovaries may impact:
- The number and quality of eggs
- The process of ovulation, making it irregular or less efficient
- The fallopian tubes, which may become swollen or partially blocked, preventing the egg and sperm from meeting
Chronic inflammation from endometriosis leads to scar tissue (adhesions) that can cause pelvic organs to stick together. This can:
- Block or distort the fallopian tubes, preventing fertilization
- Make it difficult for a fertilized egg to travel to the uterus
- Disrupt the shape and function of the uterus, which may affect embryo implantation
The presence of abnormal tissue causes a state of ongoing inflammation in the pelvic cavity. This inflammatory environment:
- Damages egg and sperm cells
- Interferes with fertilization
- Can impair the development and quality of the embryo
Endometriosis is an estrogen-driven condition that can create hormonal imbalances in the body. This may:
- Alter the timing of ovulation
- Affect the thickness and quality of the uterine lining
- Reduce the chances of successful embryo implantation
Can You Get Pregnant with Endometriosis?
• Mild Endometriosis = Higher Chances
Women with mild to moderate endometriosis often conceive naturally, especially if their fallopian tubes are open and ovulation is normal. In many cases, lifestyle changes, medications, or minor surgical treatment can improve fertility outcomes.
• Severe Cases May Need Surgery or IVF
Women with moderate to severe endometriosis may face more challenges. Large cysts or extensive scar tissue might require:
- Laparoscopic surgery to remove endometriosis lesions and adhesions
- IVF (In Vitro Fertilization) to bypass damaged tubes or improve egg-sperm interaction in a controlled lab setting
The good news is that treatment—whether medical or surgical—can significantly improve fertility. Many women can conceive naturally within 6 to 12 months after surgery or therapy.
At Isha Women’s Hospital, under the guidance of Dr. Chinmay Pataki, the best fertility expert and laparoscopic surgeon in Thane, many couples have successfully overcome endometriosis-related infertility and welcomed healthy pregnancies.
If you’ve been diagnosed with endometriosis and are trying to conceive, the good news is—
There are several ways to manage your condition and boost fertility. From natural approaches to advanced fertility treatments, a combination of methods can help you take control of your reproductive health.
Natural Ways to Manage Endometriosis
• Anti-Inflammatory Diet
- Eating the right foods can lower inflammation levels in the body. Include:
- Leafy greens, colourful vegetables, and berries rich in antioxidants
- Omega-3 fatty acids from walnuts, flaxseeds, and fish
- Turmeric, a natural anti-inflammatory spice
- Avoid processed foods, sugar, and red meat, which may worsen symptoms
Regular movement helps reduce pelvic pain, improves blood circulation, and supports hormone balance. Gentle yoga poses and low-impact exercises can also ease stress and tension in the pelvic region.
• Stress Management
Chronic stress can increase inflammation and worsen hormonal imbalances. Practices like deep breathing, meditation, journaling, or talking to a counsellor can support mental and physical well-being.
• Supplements
Some supplements may improve symptoms and support reproductive health:
- Omega-3 fatty acids for anti-inflammatory effects
- Magnesium to ease cramps and muscle tension
- NAC (N-acetyl cysteine), shown to help reduce endometrial lesions
Being overweight or underweight can affect hormone levels and ovulation. A balanced lifestyle and a healthy weight range can significantly improve fertility outcomes.
Medical & Surgical Treatments
1. Medications
- Hormonal Birth Control: Helps manage pain and reduce the growth of endometrial tissue.
- GnRH Agonists: These medications suppress estrogen production, which slows or stops the progression of endometriosis.
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Provide pain relief for menstrual cramps and pelvic discomfort.
2. Surgery
Laparoscopy is the gold standard for both diagnosis and treatment. During this minimally invasive procedure, a surgeon removes or destroys visible endometrial lesions and scar tissue.
This improves fertility by restoring normal pelvic anatomy and removing blockages that prevent egg-sperm interaction or embryo implantation.
3. Fertility Treatments
If natural conception is difficult, fertility treatments offer promising options:
- Ovulation Induction with Timed Intercourse: Stimulates egg release and times intercourse to improve chances of conception.
- IUI (Intrauterine Insemination): Places sperm directly into the uterus during ovulation, bypassing potential barriers caused by endometriosis.
- IVF (In Vitro Fertilization): Recommended for women with moderate to severe endometriosis. IVF allows fertilization outside the body, bypassing fallopian tube blockages and increasing success rates.
- Early diagnosis and treatment are key
- Lifestyle changes and medical care can significantly improve fertility
- Advanced treatments like IVF offer hope for even the most complex cases
Your dreams of motherhood are possible. Let us help you make them a reality.
Frequently Asked Questions (FAQs)
Ans - Yes—many women with endometriosis do conceive, naturally or with help.
2. What stage of endometriosis causes infertility?
Ans - Stage 3 and 4 are more likely to impact fertility, but even mild cases can interfere.
3. Does surgery improve fertility in endometriosis?
Ans - Yes—laparoscopy can significantly boost fertility outcomes in many women.
4. Can endometriosis affect IVF success?
Ans - Yes, but IVF is often effective, especially after treating endometriosis.
5. What foods should I avoid with endometriosis?
Ans - Avoid processed foods, dairy, red meat, caffeine, and alcohol—they worsen inflammation.
