Ovarian Cysts: Symptoms, Treatment & Prevention
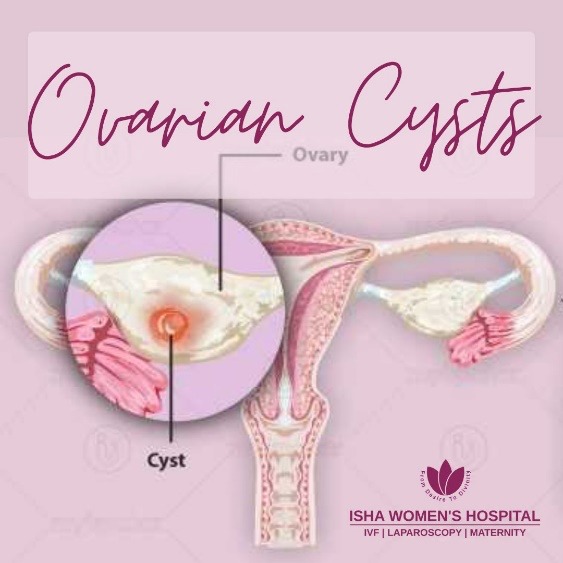
What Are Ovarian Cysts?
Types of Ovarian Cysts:
These cysts form as a natural part of the menstrual cycle and are usually not dangerous.
- Follicular Cyst: During ovulation, a small sac (called a follicle) holds the egg, if the follicle doesn’t open and release the egg, it can grow into a cyst. This is usually painless and disappears in a few weeks.
- Corpus Luteum Cyst: After the egg is released, the empty follicle becomes a structure called the corpus luteum. Sometimes, it fills with fluid or blood and becomes a cyst. It may cause pain or bleeding but often goes away on its own.
Functional cysts are the most common and usually resolve without treatment.
2. Dermoid Cyst (Also Called Mature Cystic Teratoma)
- This cyst develops from embryonic (baby-like) cells, so it can contain strange things like hair, teeth, or skin tissue.
- They are usually benign (non-cancerous).
- Can grow large and may need surgical removal.
Often found in younger women and may be discovered during a routine check-up or scan.
3. Endometrioma (Chocolate Cyst)
- Found in women who have endometriosis—a condition where the lining of the uterus grows outside it.
- These cysts are filled with old, dark brown blood, which is why they're nicknamed “chocolate cysts”.
- They can cause painful periods, pain during sex, and affect fertility.
Requires medical management or sometimes laparoscopic surgery.
4. Cystadenoma
- These cysts develop from the outer surface of the ovary.
- They can be filled with watery (serous) or thick, mucous-like fluid (mucinous).
- They can grow very large and may cause pressure or bloating in the abdomen.
Often need surgical removal if they grow big or cause discomfort.
5. Polycystic Ovaries (Seen in PCOS)
- In Polycystic Ovary Syndrome (PCOS), the ovaries produce many tiny, immature cysts.
- These are not harmful on their own, but they are a sign of hormonal imbalance.
- PCOS can cause irregular periods, acne, weight gain, and difficulty getting pregnant.
Needs long-term management with lifestyle changes, medications, and hormonal therapy.
What Causes Ovarian Cysts?
1. Ovulation (Most Common Cause): Every month, the ovaries release an egg. If the follicle (the sac that holds the egg) doesn’t open or doesn't dissolve after releasing the egg, it can form a functional cyst. This is normal and usually goes away on its own.
2. Hormonal Imbalances: Conditions like Polycystic Ovary Syndrome (PCOS) or thyroid disorders can lead to hormonal changes that prevent regular ovulation. This can cause multiple small cysts to develop in the ovaries. PCOS is a major cause of multiple ovarian cysts and fertility issues.
3. Endometriosis: In endometriosis, the tissue that lines the uterus grows outside of it—even on the ovaries. This can lead to blood-filled cysts called endometriomas or “chocolate cysts,” which can be painful and affect fertility.
4. Pelvic Infections: Severe pelvic infections can spread to the ovaries and cause pus-filled cysts or abscesses. These are serious and require immediate treatment.
5. Previous Ovarian Cyst History: If you've had ovarian cysts before, you're more likely to develop them again—especially if the root cause hasn’t been treated.
6. Genetic or Embryonic Cells (Dermoid Cysts): Some cysts, like dermoid cysts, form from embryonic cells and can contain tissues like hair or teeth. These are not caused by hormones and may be present from birth, growing over time.
Common Symptoms of Ovarian Cysts
- Pelvic pain (dull or sharp)
- Bloating or fullness
- Pain during intercourse
- Menstrual irregularities
- Frequent urination or difficulty emptying the bladder
- Sudden, severe abdominal pain (in case of rupture or torsion)
At Isha Women’s Hospital, Dr. Chinmay Pataki, the best gynecologist conducts timely ultrasounds and diagnostic tests to ensure early detection and proper management.
Diagnosis & Treatment Options
Let’s explore how ovarian cysts are diagnosed and treated.
How Are Ovarian Cysts Diagnosed?
Detecting ovarian cysts early ensures timely and effective treatment. Here's how doctors identify them:
- Pelvic Examination
A routine check where the doctor feels the ovaries for any unusual swelling or mass. - Ultrasound Scan
A painless imaging test that shows the size, shape, location, and type of cyst (fluid-filled or solid). - Blood Tests (CA-125)
In cases of complex or persistent cysts, a CA-125 test may be done to check for markers related to ovarian cancer. - Laparoscopy
A minimally invasive procedure where a tiny camera is inserted through a small cut in the abdomen to view the cyst directly. It also allows for cyst removal if needed.
Treatment Options for Ovarian Cysts
Not all cysts need treatment. The choice depends on the type, size, symptoms, and your age or fertility goals.
- Watchful Waiting: In many cases, cysts go away on their own within a few weeks or months. Your doctor may recommend monitoring with regular ultrasounds.
- Medications:
Painkillers: For managing cramps or abdominal discomfort.
- Surgical Treatment: Surgery is considered if:
Laparoscopy: Minimally invasive, used for small and benign cysts.
Dr Chinmay Pataki is the best laparoscopic gynec surgeon renowned for his surgical expertise to provide quick recovery time and minimal scars to patients with complete cure to their reproductive health.
When Should You See a Doctor?
- Severe pelvic or abdominal pain
- Unusual bloating or swelling
- Heavy or irregular menstrual bleeding
- Fainting, dizziness, or weakness (could indicate a ruptured cyst)
Prevention & Lifestyle Tips
How to Prevent Ovarian Cysts Naturally
- Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
- Include fiber to help eliminate excess hormones naturally.
- Avoid processed foods, sugary snacks, and trans fats that disrupt hormonal balance.
- Regular physical activity helps your body regulate insulin and reproductive hormones.
- Maintaining a healthy weight is especially important for women with PCOS or irregular cycles.
3. Reduce Stress & Improve Sleep
- Chronic stress can disrupt your body’s hormonal signals, potentially triggering cysts.
- Practice yoga, meditation, or deep breathing to manage stress effectively.
- Ensure 7–8 hours of quality sleep each night to support overall hormonal health.
- Routine gynecological check-ups help in the early detection of ovarian cysts or related conditions.
- Pelvic ultrasounds and hormone testing can alert your doctor to any developing issues early on.
At Isha Women’s Hospital, under the leadership of Dr. Chinmay Pataki—the best gynecologist in Dombivali, top fertility specialist, and the only male fertility expert in the entire Thane district—you’re in the safest hands. Isha Women Hospital is recognized as the best fertility centre in Thane, offering cutting-edge treatments with a personal touch.
Don’t wait for symptoms to worsen. Invest in your health today—because a healthier you is a happier you.
Visit Isha Women’s Hospital—where hope begins and health thrives.
Frequently Asked Questions (FAQs)
Ans - Most are harmless, but large or ruptured cysts can cause complications.
2. Can birth control pills prevent ovarian cysts?
Ans - Yes, they help regulate ovulation and reduce cyst formation.
3. Do ovarian cysts affect fertility?
Ans - Some cysts, like PCOS-related or endometriomas, may affect fertility.
4. Can ovarian cysts go away on their own?
Ans - Yes, functional cysts often disappear within a few months.
5. How do I know if an ovarian cyst has ruptured?
Ans - Symptoms include severe pelvic pain, bloating, dizziness, and nausea. Seek medical attention immediately.
